On a sweltering morning in Watts, community health worker Elizabeth Calvillo rapped on a shut gate with her pen, hoping the sound would carry over the rumble of an airplane.
“Good morning! ¡Buenos días!”
When a young mother emerged from the house in her pajamas, shading her eyes from the sun, Calvillo and co-worker Maria Trujillo explained they were knocking on doors to see if she or her neighbors needed anything. They asked the mother: Was she on Medi-Cal? Was there anything else she needed?
The 26-year-old said she had insurance but was tired of spending hours to get seen at a downtown clinic that said it would take months to schedule a physical for her 3-year-old daughter.
“I haven’t even gotten my checkups because it’s so hard to get an appointment,” the woman lamented.
The two promptly offered to refer her to a local clinic. Trujillo put in the referral electronically on the spot. Calvillo told her they would follow up in a week or two to make sure she had gotten an appointment.
The mother thanked them. “I’ve been stressing about it. You guys came at the right time!”
“That’s what we’re here for,” Calvillo replied.
1
2

1. Elizabeth Calvillo, left, and Maria Trujillo go door to door in Watts trying to connect people with healthcare and other services. 2. Calvillo, left, and Trujillo speak with Brenda Montes, 26, in Watts on a recent canvassing of the neighborhood. (Dania Maxwell / Los Angeles Times)
In Los Angeles County, the public health department is trying to — quite literally — meet people where they are. This year, it has launched a pilot project that sends teams to knock on doors in neighborhoods like Watts, Pacoima and Lincoln Heights to ask residents what they need.
The county might be able to reach people with billboards or ads, X or Instagram, but knocking on doors is “more personal,” said Trujillo, a community health worker with Children’s Institute, one of the local groups carrying out the work. “You have an actual person coming and showing that they want to be of service to you.”
The Community Public Health Teams, run by community organizations and health groups in partnership with the county, are each tasked with knocking on anywhere from 8,000 to 13,000 doors in designated areas.
Community health workers ask questions for a household assessment — which covers unmet needs for medical care, assistance needed for day-to-day activities, mental health, housing instability, neighborhood violence and other issues — and try to connect people with services such as enrolling in Medi-Cal or finding a food bank. Each team is also linked to a healthcare partner that can offer primary care.
“This is bringing healthcare to the door of the individual,” said Monica Dedhia, director of community health programs for Children’s Institute, “versus waiting for someone to make an appointment.”
The pilot program is expected to last five years, with teams returning at least once a year to check on households. Tiffany Romo, director of the community engagement unit at L.A. County Public Health, likened it to “concierge service.” Even after someone has been linked with healthcare or other needed services, she said, the teams will reach out to them again, making sure they actually got what they needed.
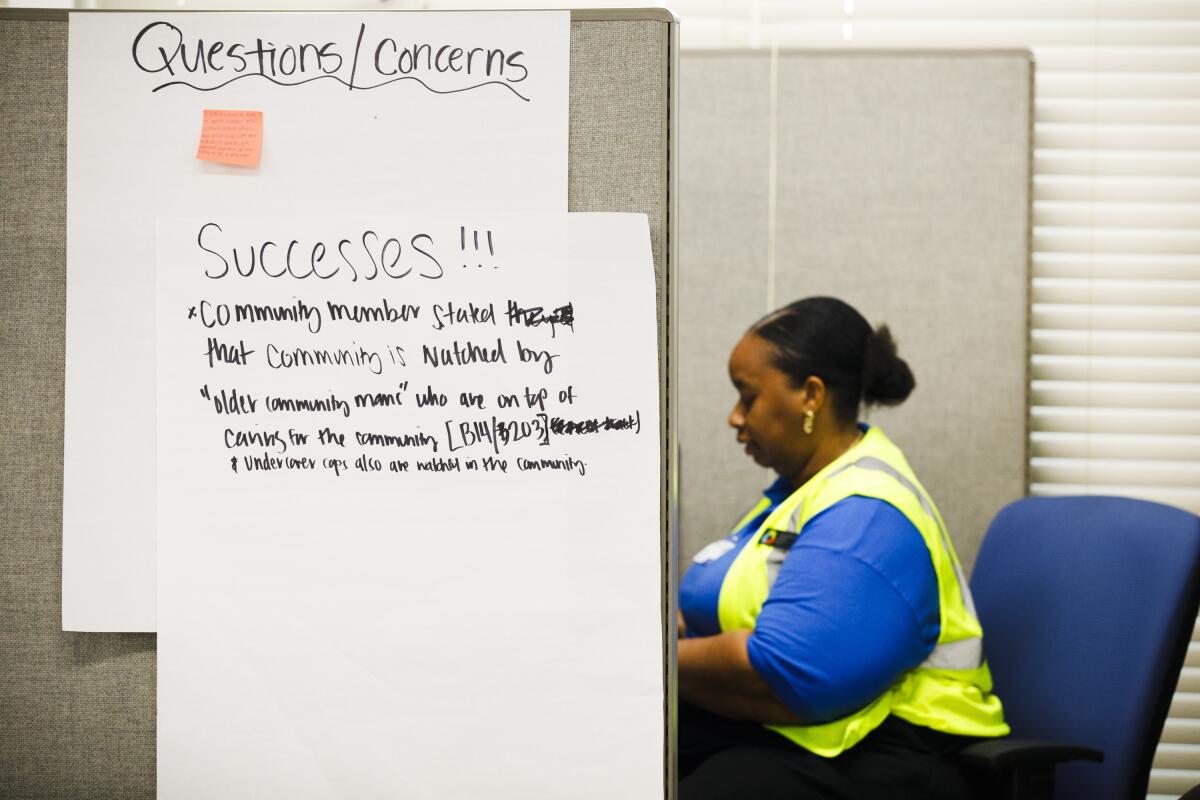
Ashley Jackson works in the Pacoima office of Providence’s Community Public Health Team, where “successes” are listed on a poster.
(Carlin Stiehl / For The Times)
It is a system more common in countries like Costa Rica and Cuba, credited with forging closer connections between health agencies and their communities. Costa Rica, which sends health workers to households, saw a drop in potential years of life lost — one that was sharper for its poorest residents than its wealthiest ones.
But it’s “rarely done in the U.S.” for health workers to be assigned responsibility for the whole population in a geographic area, “including the ones that don’t show up at clinics,” said Dr. Asaf Bitton, associate professor of medicine and healthcare policy at Harvard. “That’s a whole different orientation.”
“We know that most health is created outside the medical care system,” Bitton said, but commercial insurers do not typically pay for things like food or housing. Instead, the approach in the U.S. has largely been, “We will pay for whatever you need once you have the heart attack.”
The pilot program relies on $75 million from a federal grant that will be spread out over five years, providing $1.5 million to each team in 10 “high need” areas.
What success looks like under the program, Romo said, “is really up to the community to define.” But public health officials say their hope is it will drive down inequities and result in healthier neighborhoods. Analyzing the information it gathers will also help inform future efforts at the public health department.
L.A. County Public Health Director Barbara Ferrer said the pilot program emerged not only out of the successes seen in Costa Rica and Cuba, but out of the experiences of the COVID-19 pandemic, when it “became abundantly clear, particularly in lower resource communities, that people were very disconnected from services and support.”
In many cases, “it wasn’t that they were necessarily uninsured or underinsured,” Ferrer said. “They just weren’t connected to a healthcare provider” or other local services. Sometimes the problem was “an information gap,” sometimes fear or distrust and sometimes barriers like long waits or burdensome paperwork, she said.

Providence’s Community Public Health Team is reflected in a mirror in Pacoima.
(Carlin Stiehl / For The Times)
In Pacoima, a working-class neighborhood in the San Fernando Valley, many “people just don’t know those resources are available,” said Dionne Zantua, program manager for another team run by Providence Health & Services Foundation.
Scarlett Diaz, a Providence community health worker, said many Pacoima residents also fear that signing up for programs such as Medi-Cal could jeopardize their chances of a green card or citizenship, even as California officials have thrown open the program to eligible residents regardless of immigration status.
Misinformation isn’t the only obstacle: As Diaz and her co-worker Ashley Jackson rounded the neighborhood one Wednesday, clipboards in hand, they faced locked gates and growling dogs. Some residents waved them off or told them to come back another time.
But their daily rounds have made a difference. Before the Providence team in their neon vests stopped at her gate, Monica Avila said she had already seen them walking her Pacoima neighborhood. The 62-year-old tried to hush her barking dogs as Diaz and Jackson began asking about anything she needed.
Avila told them about the speed bumps she wanted the city to install on her block. She told them her husband had died and one of her sons had been killed. That she used to go out dancing, but not anymore.
She told them about the anxiety she suffered, “bad anxiety where like I feel like I’m being locked in,” so bad it was hard to stop by a community center for free resources. Diaz gave Avila her number, offering to help her get what she needed there next time without having to join the crowd inside.

Ashley Jackson of Providence’s Community Public Health Team speaks with Monica Avila in Pacoima last month.
(Carlin Stiehl / For The Times)
Avila seemed relieved. “Thank you for coming and listening to me,” she said.
The work can be slow going: After stopping at more than 40 homes that morning, Jackson and Diaz had ultimately completed two assessments with residents. They left door hangers about the project on fences, planning to return to people they hadn’t reached.
Romo said she expects that a major challenge will be simply getting people to open their doors. Dedhia said that in Watts, for instance, the community “has been heavily surveyed, but the follow-up isn’t necessarily there all the time.” Another community health worker in Watts recalled that at one home, a man grew angry when the team stopped by, asking them, “Isn’t it obvious what the community needs?”
But Ferrer said the program hinges on the fact that “a lot of people have things that they need help with — and they’re not getting help.”
“We’ll build trust very quickly,” she said, “if we can deliver on that.”


